ACTH - New perspective to Hypertension and adrenal function
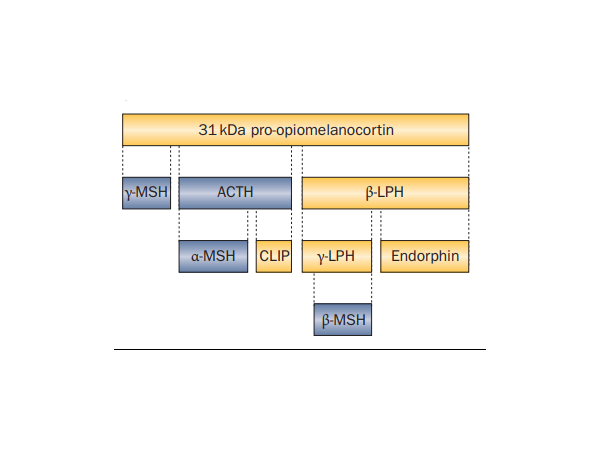
Adrenocorticotropic hormone (ACTH) is a polypeptide hormone secreted by the anterior pituitary gland and synthesized from the precursor pro-opiomelanocortin (pre-POMC). Pre-POMC translates into a 241-amino acid polypeptide after removing the signal peptide, which then undergoes a series of modifications (such as phosphorylation and glycosylation) before being hydrolyzed by endopeptidase to form polypeptide fragments with different physiological activities. Among them, residues 138-176 constitute ACTH, with a molecular weight of 4540 Da.
ACTH and the HPA Axis
ACTH is a crucial component of the hypothalamic-pituitary-adrenal (HPA) axis and is often produced during biological stress. In the normal HPA axis, the secretion of ACTH is regulated by corticotropic hormone releasing hormone (CRH). ACTH, in turn, stimulates the adrenal cortex to secrete cortisol and androgens, which are also negatively feedback-regulated by serum cortisol concentrations. Additionally, the secretion of ACTH exhibits a circadian rhythm pattern, with a peak at 6-8 am and a trough at 10 pm to midnight [1] [2].

Clinically, elevated ACTH levels are commonly seen in primary adrenocortical hypofunction, congenital adrenocortical hyperplasia, ectopic ACTH syndrome, and ectopic CRH tumor. Additionally, ACTH can be used as an indicator for monitoring treatment response, prognosis, and outcome in ectopic ACTH syndrome. Decreased ACTH levels are commonly observed in hypopituitarism, primary adrenocortical hyperfunction, and iatrogenic Cushing's syndrome. ACTH, combined with other markers, can be used to differentiate adrenocortical hyperfunction and hypofunction.
Blood ACTH combined with cortisol testing can help diagnose various conditions. ACTH stimulates the production of cortisol. When adrenal cortisol secretion is excessive, it can lead to metabolic disorders and decreased resistance to infection, triggering Cushing's syndrome. ACTH levels exceeding 200 pg/mL usually indicate ectopic ACTH production. If ACTH levels in patients with Cushing's syndrome are lower than normal, adrenal adenomas or carcinomas may be the cause of hyperfunction. If patients have elevated ACTH and decreased cortisol, it may be Addison's disease. In addition, various diseases caused by HPA axis dysregulation can also lead to secondary and primary hypertension. ACTH and cortisol are positively correlated with systolic and diastolic blood pressure and belong to the five hormones related to hypertension, which are of great significance for the diagnosis of hypertension.
Some studies have shown that ACTH has potential therapeutic effects on nephrotic proteinuria. ACTH can induce the remission of proteinuria symptoms and protect the kidneys through various regulatory mechanisms. These mechanisms include ACTH regulating cortisol production, which then suppresses immune responses and has anti-inflammatory effects; melanocortin receptors (MCRs) directly mediating systemic immune regulation and antigenic effects, with MRCs mediating direct protective effects on renal cells, especially podocytes; and hepatocyte MCRs mediating the correction of lipid abnormalities to exert renal protective effects [4].
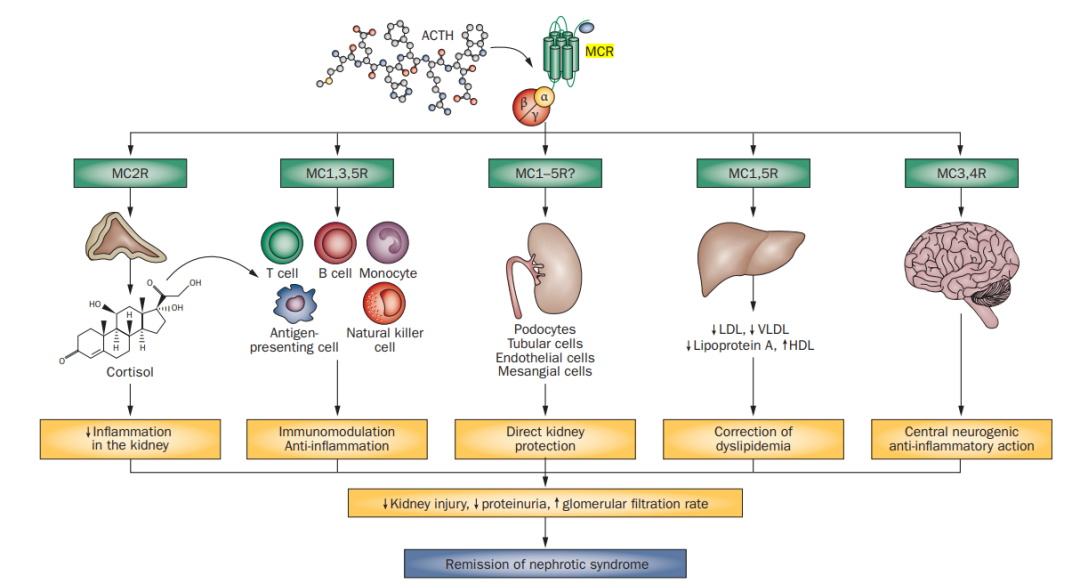
The potential mechanism of ACTH in the treatment of nephrotic proteinuria
The common method for detecting ACTH is the immunoassay method. However, since ACTH and cortisol concentrations are related to the circadian rhythm, the time of patient blood sample collection is an important determinant of the efficacy of plasma ACTH testing. Combining it with simultaneously measured serum cortisol often allows for the best interpretation of the results. When evaluating patients with adrenal insufficiency, testing should be performed in the morning whenever possible, as plasma ACTH and serum cortisol concentrations are typically at their peak at this time. However, when urgently evaluating patients with potential adrenal insufficiency (such as in an intensive care unit or emergency room), blood samples should be collected at any time before glucocorticoid therapy is administered.
Starter Bio High sensitivity ACTH recombinant antibody
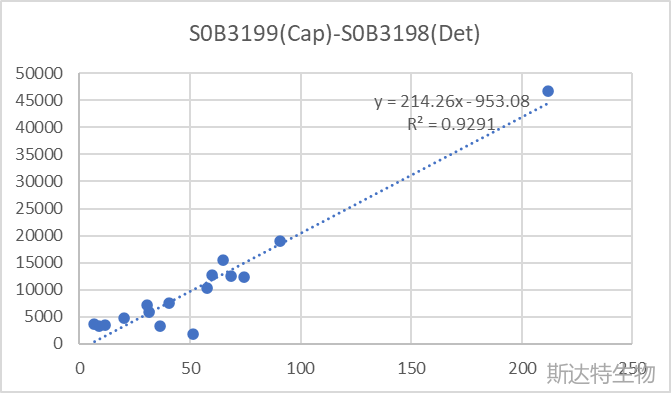
S-RMab® ACTH recombinant antibodies on chemiluminescent immunoassay (CLIA) platform has demonstrated excellent detection linearity and sensitivity down to 10 pg/ml or lower when tested against Roche quality control samples. Further optimization of the assay could potentially improve sensitivity even further.
S-RMab® recombinant mAbs
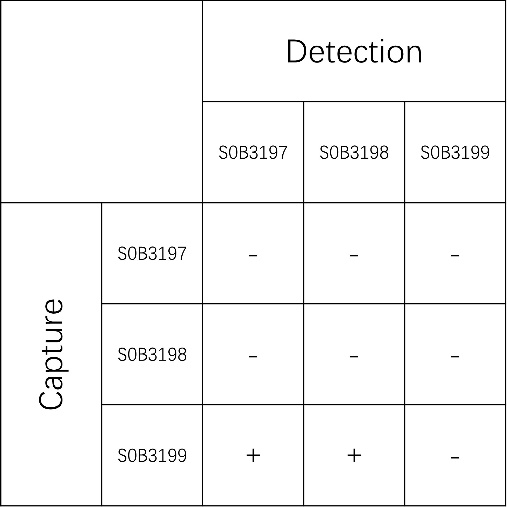
Paired Antibody:
S0B3199(Capture) - S0B3197(Detection)
S0B3199(Capture) - S0B3198(Detection)
Reference
[1] Dibner C , Schibler U , Albrecht U .The mammalian circadian timing system: organization and coordination of central and peripheral clocks.[J].Annual Review of Physiology, 2010, 72(1):517-549.DOI:10.1146/annurev-physiol-021909-135821.
[2] Russell, G., Lightman, S. The human stress response. Nat Rev Endocrinol 15, 525–534 (2019).
[3] National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
[4] Gong, R. The renaissance of corticotropin therapy in proteinuric nephropathies. Nat Rev Nephrol 8, 122–128 (2012).
Product Information
| Gatalog Num | Product Name | Product Parameters | Price |
| S0A4040 | Rat IL-6, His tag | Host : Rat | $220 |
| Expression System : HEK293 | |||
| S0B3198 | ACTH Recombinant Rabbit mAb (SDT-362-51-2) | Host : Rabbit | $350 |
| Conjugation : Unconjugated | |||
| S0B3197 | ACTH Recombinant Rabbit mAb (SDT-362-51) | Host : Rabbit | $350 |
| Conjugation : Unconjugated | |||
| S0B3199 | ACTH Recombinant Rabbit mAb (SDT-363-92) | Host : Rabbit | $350 |
| Conjugation : Unconjugated |




